Abstract
Study design: Questionnaire.
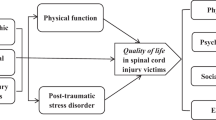
Objective: To evaluate the prevalence of post-traumatic stress disorder (PTSD) and emotional distress in persons with recent onset of spinal cord lesion.
Setting: Denmark.
Methods: A total of 69 patients with paraplegia or tetraplegia from two rehabilitation centres in Denmark filled in the questionnaire. PTSD and emotional distress were assessed using the Harvard Trauma Questionnaire and the Medical-Based Emotional Distress Scale, 83 days on average after the spinal cord lesion. The level of neurological lesion and completeness were recorded adhering to the International Standards for Neurological Classification of Spinal Cord Injury.
Results: The prevalence of PTSD was 20%. Patients with PTSD experienced significantly more symptoms of depression and more emotional distress than patients without PTSD. Age and neurological level were related to PTSD in patients with traumatic injuries, but not in patients with nontraumatic lesions.
Conclusions: Persons with a recent onset of spinal cord lesions are at increased risk of having PTSD, and comorbidities such as depression and other symptoms of emotional distress.
Similar content being viewed by others
Introduction
A spinal cord lesion (SCL) can be viewed as a traumatic event that is accompanied by a number of losses. The individual has to cope with physical problems, with paralysis, bladder, bowel, and sexual dysfunctions, and also with the impact that the SCL has on his/her social life. Hence, coping with SCL requires considerable resources, the absence of which can result in a variety of pathological reactions.1,2 One such pathological reaction is post-traumatic stress disorder (PTSD), which is different from depression because the trigger is included in the diagnostic criteria of PTSD.3 The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) defines PTSD as ‘the development of characteristic symptoms following exposure to an extreme traumatic stressor’.3 In addition to the 1-month time criterion, two further criteria have to be met. The person must have experienced, witnessed, or been confronted with an event/events that involved death or the threat of death, or a threat to the physical integrity of self and others (criterion Al). The person's response has to involve intense fear, helplessness, or horror (criterion A2).3 Additionally, at least one in five symptoms of re-experiencing, at least three in seven symptoms of avoidant/numbing, and at least two in five symptoms of increased arousal have to be met.3
In a review conducted by Kennedy and Duff,4 the prevalence of PSTD after SCL is found to be 10–40%. A very high prevalence of PTSD is found in children with SCL, ranging from 25 to 33%,5,6 and almost 16% of SCL veterans who have been exposed to combat experience are current diagnosed with PTSD, while none of the nonwar veterans met the diagnostic criteria for current PTSD.7 In addition, considerably fewer tetraplegics than paraplegics are reported to suffer from PTSD.8,9 Biological or physiological determinants may contribute to the differences in psychological reactions.8,9,10 High rates of comorbidity between PTSD and depression have been reported in female victims of partner violence, as well as in Israeli and Vietnam veterans.11,12,13 Furthermore, depression has been found to be the most common comorbid disorder in victims of fire and motor vehicle accidents diagnosed with PTSD.14 In a review conducted by Boekamp et al,15 the incidence of depression after SCL is found to be between 20 and 45%. Women are estimated to have a higher prevalence rate of depression (47%) after SCL compared with men (25%).16 Few studies have investigated the level of comorbidity between PTSD and depression in persons with SCL. One such study found strong associations between post-traumatic distress symptoms and de-pression in 85 in-patients with SCL.17
The aim of the present study was to determine the prevalence of PTSD in patients with new SCL. The hypotheses to be tested were as follows: (1) Patients with traumatic SCL suffer more from PTSD compared with those with nontraumatic SCL; (2) Patients with SCL suffering from PTSD have higher levels of depression and emotional distress compared with those without PTSD; (3) There exist positive associations between PTSD and depression, and between PTSD and emotional distress; (4) Injury severity (paraplegia/tetraplegia and neurological level) influences PTSD severity for patients with nontraumatic and traumatic lesions.
Materials and methods
Sample
A total of 85 patients, with new SCL, admitted to two rehabilitation centres for SCL in Denmark between March 2000 and July 2001, were invited to participate. Of these, 16 patients refused to participate, 11 of the 16 refused because they felt the questionnaire could cause further psychological distress, the remaining five patients did not give any reason as to why they would not participate. Thus, the final sample consisted of 69 (81%) patients. Inclusion criteria were as follows: only patients who were newly injured, had permanent neurological loss, were at least 18 years of age, had no head injuries, or other disabilities except the SCL, and were able to speak Danish were included.
Patients were informed orally and in writing about the study, and were asked to return a written form of con-sent. The study was approved by an ethics committee and the Helsinki Declaration was respected.
Procedure
In order to minimize any emotional distress caused by the questionnaire, collaboration between the psychologists at the rehabilitation centres and the researcher was maintained. The psychologists, however, had no knowledge of any of the responses to the questionnaire.
Measures
Patients were given a purpose-designed questionnaire that included questions on educational level, occupation, and marital status. Date of birth, date of lesion, date of admission to the rehabilitation centre, event leading to SCL, and level of neurological lesion and completeness were taken from medical records. Level of neurological lesion and completeness were recorded according to the International Standards for Neurological Classification of Spinal Cord Injury.18 In compliance with these standards information as to whether the patient was a tetraplegic or a paraplegic, and whether the lesion was complete or incomplete was recorded.
To assess PTSD severity, patients were asked to complete the Harvard Trauma Questionnaire (HTQ),19 section IV. The HTQ was chosen because it is a self-report scale referring to the specific trauma experienced by the respondent. Sixteen of the 30 symptom items (the PTSD-score) correspond to the Diagnostic and Statistical Manual of Mental Disorder3 (DSM-III-R and DSM-IV) diagnosis of PTSD.20,21 The symptoms are rated on a four-point Likert scale ranging from ‘not at all’ to ‘most of the time’. Two measures of PTSD make different statistical procedures possible. (1) The PTSD score is the sum of items 1–16 divided by 16.19 (2) In addition, differentiation between diagnostic levels of PTSD is possible.20 The algorithm for caseness includes a positive response (3 or 4) on at least one of the four re-experiencing symptoms (criterion B), on at least three of the seven avoidance/numbing symptoms (criterion C), and at least two of the five arousal symptoms (criterion D).22
The Medical-Based Emotional Distress Scale (MEDS)23 was used to assess depression. This instrument is developed specifically to assess the type and severity of emotional distress following a physical illness, injury, or disability. In order to prevent confusion between physical symptoms derived from SCL and physical symptoms derived from a potential depression, the MEDS focuses on cognitive and emotional factors of depression, and avoids the use of somatic symptoms. The MEDS was originally designed to be administered as a structured interview, but is used as a self-report measure in the present study. A total MEDS score correlates significantly with other distress and depression measures, that is, the Symptom Checklist-90-Revised (r=0.77), the Zung Self-Rating Depression Scale (r=0.71), and the Rosenberg SE Scale (r=−0.75).23 The MEDS includes seven subscales: dysphoria (eight items), irritability (nine items), anhedonia (11 items), social withdrawal (nine items), rumination over past events (six items), cognitive perspective in the present (eight items), and expectations for the future (nine items). Two different 5-point scales are used. One quantifies the frequency of different emotional reactions ranging from ‘never’ (0) to ‘always present’ (4), and one rates the intensity of emotions that occurred ranging from ‘not present’ (0) to ‘very much present’ (4). The internal consistency for the total MEDS score is 0.92, and all subscales show moderately high internal consistency.23
Data analysis
Prior to analyses and following Tabachnick and Fidell,24 data were examined for accuracy of data entry, missing values, and fit between their distributions. All the assumptions for multivariate analysis were met. Data were screened for normality, and found to be normally distributed, thus allowing for parametric analysis. Independent samples t-test were conducted to examine differences between groups (PTSD versus no PTSD, and traumatic versus nontraumatic lesions) on PTSD and emotional distress (the seven subscales of MEDS and total MEDS score). Associations between PTSD score and the seven subscales of MEDS and total MEDS score were analysed using Pearson's product moment correlation coefficient. A linear multiple regression analysis was conducted to investigate the relation between emotional distress and PTSD, with PTSD score as the dependent variable. Only variables at P<0.001 in the correlation analyses were entered in the model. To investigate if injury severity (paraplegia versus tetraplegia and neurological level) could predict PTSD in patients with traumatic versus patients with nontraumatic lesions, two linear multiple regression analyses were carried out. Gender, age, and time since lesion were also entered in the equations.
Results
In all, 27 patients were tetraplegic and 41 were paraplegic. Data for one patient were missing. Sixty-one percent had neurologically incomplete lesions were found in 61%. At the time of assessment, patients ranged from 18 to 85 years in age (mean 48, SD 16). Time since lesion was 88 days on average (SD 67; range 20–431 days). Time from lesion to admission to the rehabilitation centre was 47 days on average (SD=62; range 2–423 days), which, for most of the patients, was the time spent in hospital. Of the patients, 44 (64%) were injured in traumatic accidents (motor vehicle accidents, falls, accidents at work, and bathing accidents) and 25 patients (36%) sustained lesions resulting from nontraumatic events (eg tumors, disc prolapses, aneurisms). The majority was well educated, 50% had more than 12 years of education, 12% had completed 12 years of education, and 38% had completed 10 years of education or less. In all, 61% were employed prior to the lesion, 6% were unemployed, 4% were studying, 26% were retired, and 3% failed to state occupation. A total of 61% were married or cohabitating.
Of the patients, 14 (20%) met the criteria for full-blown PTSD. Ignoring the criteria of 1-month needed for the diagnosis of PTSD, two more of the patients (23%) met the criteria for full-blown PTSD. In all, 12 patients (17%) displayed two of the three symptom clusters meeting the criteria for partial PTSD. Of the subjects, 38 (55%) met the criteria for re-experiencing, 21 (30%) met the criteria for avoidance, and 35 (51%) met the criteria for arousal. There was no significant difference in PTSD level between patients with traumatic SCL and those with nontraumatic SCL.
The mean score on the MEDS score for patients with PTSD was 111.8 (SD 14.4; range 88.9–131.5). The mean score on the MEDS for patients without PTSD was 91.2 (SD 15.4; range 54–123). Results showed that patients with PTSD had significantly higher mean scores on depression (total MEDS score) than patients without PTSD (t=−4.8, df=63, P=0.0005). Patients with PTSD experienced significantly more dysphoria (t=−5.2, df=65, P=0.0005), irritability (t=−4.7, df=66, P=0.0005), social withdrawal (t=−2.5, df=65, P=0.01), ruminated more over past events (t=−6.0, df=66, P=0.0005), and had fewer expectations for the future (t=2.6, df=64, P=0.01). There were no significant differences between the PTSD group and the non-PTSD group on the subscales anhedoma and cognitive perspective in the present.
The correlations between PTSD and emotional distress are shown in Table 1.
Dysphoria, irritability, rumination over past events, expectations for future events, and total MEDS score, respectively, were all statistically significant at the 0.001 level. These variables were entered in the linear regression analysis as predictor variables. The criterion variable was the PTSD score. The linear combination of emotional distress was significantly related to the PTSD score, R2=0.63, adjusted R2=0.60, F(5,59)=20.3, P=0.0005. Table 2 presents the relative strength of the individual predictors.
Evaluation of multicollinearity24 showed a condition index less than 0.30. Furthermore, no dimensions had more than one variance proportion greater than 0.50.
The linear combination of injury severity (paraplegia versus tetraplegia; complete versus incomplete), age, gender, and time since lesion was significantly related to PTSD scores in patients with traumatic SCL, R2=0.26, adjusted R2=016, F(5,37)=2.6, P=0.04, whereas the linear combination did not relate significantly to PTSD score in patients with nontraumatic SCL. Table 3 presents the relative strength of the individual predictors for the patients with traumatic SCL. Multicollinearity was not found.
Discussion
Consistent with the hypothesis, the findings suggest that SCL patients with PTSD have higher levels of depression and emotional distress (dysphoria, irritability, social withdrawal, rumination over past events, and fewer expectations for the future) than SCL patients without PTSD. Furthermore, the results showed that PTSD is associated with depression and emotional distress. Contrary to the hypothesis, there was no difference in level of PTSD between patients with nontraumatic SCL and patients with traumatic SCL. However, the linear combination of neurological level, paraplegia versus tetraplegia, age, gender, and time since injury was predictive of PTSD if the patient had a traumatic SCL, but not if the patient had a nontraumatic SCL.
In all, 20% of the patients qualified for a diagnosis of current PTSD. Disregarding the 1-month time criteria, two more of the patients fulfilled the PTSD criteria. In addition, 17% qualified for a diagnosis of partial PTSD. The prevalence of PTSD in the current study is more than twice the prevalence found in the general US population.11 Also, compared with a study of adult veterans with SCL, the prevalence rate in the present study is relatively high. Radnitz et al7,8,25 found that 11.9% of 126 male veterans with SCL met the diagnosis for current PTSD, an average of 18.8 years following lesion. Based on a survival analysis, Kessler et al11 found that two-thirds of their sample who had experienced onset of PTSD succeeded to remit. The curves decreased sharply in the first year after symptom onset. Between 1 and 6 years, the decline became more gradual.11 The present study however did not find a significant relation between prevalence of PTSD and time since lesion. On the other hand, the time span is very small in the present study compared with the study by Radnitz et al.25 The patients in the present study ranged from 20 days to almost 1 year since the time of lesion. During this time, the patients experienced a number of secondary events, including (i) severe lesion to the spinal cord, (ii) hospitalization and in some cases transfer to another hospital to undergo surgery, and (iii) transfer to a rehabilitation centre. The rehabilitation centre is for many patients remote from their place of residence, making visits from relatives and friends seldom or impossible. All of these secondary events may have an adverse effect on the patients' psychological health,26 and may account for the high occurrence of PTSD in the present sample. Yet, the prevalence of PTSD in the present study is not as high as found in other studies. Children and adolescents with SCL were found in one study to score 25.4%5 and in another study 33%6 in their prevalence of PTSD. Time since lesion in these two studies ranged from 2 months to 19 years. Care should be taken, however, when comparing children/adolescents with PTSD to adults with PTSD because several differences exist, that is, emotional numbing may often be absent in children.27
Based on the responses to the MEDS, patients with PTSD measured higher on depression than patients without PTSD. Interestingly, a number of patients without PTSD also had high scores on depression. Unfortunately, a cutoff score to distinguish those with major depression from those without, as measured by the total MEDS score, has not yet been established.23 Therefore, it is not known as to how many of the patients reach the diagnostic criteria for major depression. The present results indicate that high levels of depression occur in both patients with PTSD and in patients without PTSD, which suggests that both PTSD and depression may occur as two distinct reactions following SCL. Alternatively, depression could also have been manifest prior to the SCL. A history of psychiatric disorders has been found to predict development of depression and/or PTSD.28,29 Howell et al30 showed that six out of 22 patients with SCL received one or more psychiatric diagnoses prior to their lesion. Furthermore, Biering-Sørensen et al31 found a strong association between psychiatric illness, suicide attempts, and SCL, indicating that psychiatric disease in some cases poses a risk factor for SCL. Thus, detection of prepsychiatric illness is an important consideration in the treatment of persons with SCL.
The high occurrence of depression in patients with PTSD may also be because of a symptom overlap between PTSD diagnosis and the diagnosis of depression. One symptom in the PTSD criterion C – avoidance (loss of interest in previously enjoyed activities) – and two symptoms in criterion D – arousal (sleep problems and impaired concentration) – are symptoms that are also mentioned in the criteria for depression.3 Hence, if a person has PTSD, only two of the remaining six symptoms of depression are needed for the person to be diagnosed with depression. Kennedy and Evans17 found that depression was significantly related to intrusion and avoidance in individuals assessed 6–24 weeks after SCL. In the current study, the total MEDS score correlated significantly with the three PTSD symptom clusters and the PTSD-score. In the current study, patients with PTSD experienced higher levels of dysphoric mood, higher levels of irritability, ruminated more over past events, had fewer expectations for the future, and had a higher degree of social withdrawal compared to patients without PTSD. As shown in Table 1, some of the MEDS subscales are significantly associated to the PTSD symptom clusters and the PTSD score. For example, the MEDS subscale irritability, which may be the cognitive expression of physiological arousal, correlated significantly with PTSD arousal. Hence, a symptom overlap may account for the co-occurrence of PTSD and depression. However, anhedonia and social withdrawal, which correspond to loss of interest in previously enjoyed activities, were not found to correlate significantly with the PTSD score or the symptom cluster avoidance. This result suggests that there is no symptom overlap. Other studies32,33 have also found correlations between PTSD and depression, but their results indicated that the co-occurrence cannot be explained by the symptom overlap. Blanchard et al32 found that PTSD and depression were different disorders. When both diagnoses were met, victims of motor vehicle accidents showed more subjective distress and higher social malfunction than victims with PTSD, but not in the diagnosis of depression.32 On the basis of the multiple regression analysis, only dysphoria and expectations for the future significantly predicted PTSD controlling for all other predictors. This result indicates that being dysphoric and having lesser expectations for the future predict PTSD, thus supporting the assumption that PTSD and depression are related yet different reactions to trauma.
As in the Boyer et al study,5 the present study included patients with both traumatic and nontraumatic SCL. Distinction between these two groups showed an interesting result. The result did not show any significant difference in PTSD score between patients with traumatic SCL and those with nontraumatic lesions. However, the variables that predicted PTSD differed depending on group membership. Injury severity (paraplegia versus tetraplegia, and neurological level), age, gender, and time since lesion accounted for 26% (adjusted 16%) of the variance in PTSD in patients with traumatic lesion. For the patients with nontraumatic lesions, however, the linear combination of injury severity, age, gender, and time since lesion did not reach significance. The aetiology that led to the lesion in the spinal cord may explain the difference between the two groups. Individuals with traumatic lesions will suffer their lesion in a split second, while individuals with nontraumatic lesions may become worse over time, eventually becoming paralysed. This gradual worsening of physiological health may start an anticipatory grief reaction34 even before something has happened, and may form a safeguard against the impact of the paralysis. Individuals with traumatic SCL do not have this option. This raises a methodological limitation in the current study. The Harvard Trauma Questionnaire, which measures PTSD, refers to the event experienced by the respondent that leads to SCL. Thus, difficulties may arise for the patients with nontraumatic lesions, they may not have one single event that they can refer to. However, several of the patients in the current sample stated that their SCL was caused by a traumatic event, when in fact it was not, that is, one man linked the SCL with a fall, but the medical record stated that the SCL was a prolapse and therefore nontraumatic. Others had developed SCL after an operation, and even though they probably knew the risks of the operation, no one had expected to be paralysed. Hence, the SCL may be linked to the operation.
The bivariate correlation between the PTSD score and neurological level suggested that the patients with traumatic complete SCL have a higher risk of developing PTSD, than patients with traumatic incomplete injuries. Findings that individuals with tetraplegia have significantly less severe PTSD symptoms compared with a control group, while individuals with paraplegia do not significantly differ from these controls, have provided an argument that the nerve fibres responsible for the sympathetic arousal that accompanies PTSD may be impaired in tetraplegics, hence protecting them from experiencing the arousal symptoms.9 The results of the current study do not support this. A negative association was found between age and PTSD, indicating that higher age may mitigate against the development of PTSD after SCL.
The present study has a number of methodological limitations. The self-report measures that are used to quantify PTSD and depression may not be as sensitive as diagnostic clinical interviews. The assessment of depression in people with SCL is demanding. Distinguishing between medical and physiological conditions related to SCL and somatic symptoms as a result of a depression may be difficult as symptoms secondary to the SCL may elevate depression scale scores.35 In order to avoid this, the MEDS was chosen. The MEDS is especially developed to measure depression in persons with SCL.23 However, the MEDS has never been used as a self-report measure, which may bias the validity of the results. Validating the instrument as a self-report measure against clinical interviews could be an important step. As for now, the use of MEDS as a self-report instrument causes a significant flaw in the study. Therefore, results should be interpreted with care. Furthermore, there may be a selection bias in that not all patients at the rehabilitation centres had the opportunity to participate in the study. The staff psychologists selected which patients could participate. Furthermore, 16 subjects refused to participate, many because they felt that the questionnaire might cause further psychological distress. It is likely that patients who did not participate were more traumatized than those who participated.36 This however would have led to a deflation, rather than inflation, in the prevalence of PTSD in the current study. Despite these limitations, the present study suggests that the prevalence of PTSD shortly after SCL is considerable. In addition, a strong association between PTSD and depression was found. Future research should investigate this association with tests that are not confounded by somatic symptoms. This could clarify whether PTSD and depression are reactions to the traumatic event or if depression constitutes a predisposing factor for developing PTSD following SCL.
References
Craigh AR, Hancock KM, Dickson HG . A longitudinal investigation into anxiety and depression in the first two years following a spinal cord injury. Paraplegia 1994; 32: 675–679.
Kennedy P, Rogers BA . Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil 2000; 81: 932–937.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Vol. 4, text revision (DSM IV, TR). APA: Washington, DC 2000.
Kennedy P, Duff J . Post traumatic stress disorder and spinal cord injuries. Spinal Cord 2001; 39: 1–10.
Boyer BA et al. Prevalence and relationships of posttraumatic stress in families experiencing pediatric spinal cord injury. Rehabilitation Psychol 2000; 45: 339–355.
Boyer BA, Tollen LG, Kafkalas CM . A pilot study of posttraumatic stress disorder in children and adolescents with spinal cord injury. SCL Psychosocial Process 1998; 11: 75–81.
Radnitz CL, Schlein IS, Hsu L . The effect of prior trauma exposure on the development of PTSD following spinal cord injury. J Anxiety Disorders 2000; 14: 313–324.
Radnitz CL et al. A comparison of posttraumatic stress disorder in veterans with and without spinal cord injury. J Abnormal Psychol 1998; 107: 676–680.
Radnitz CL et al. Posttraumatlc stress disorder in veterans with spinal cord injury: trauma-related risk factors. J Traumatic Stress 1998; 11: 505–520.
Binks TM, Radnitz CL, Moran AI, Vinciguerra V . Relationship between level of spinal cord injury and posttraumatlc stress disorder symptoms. In: Yehuda R, McFarlane AC (eds). Psychology of PTSD. Annals New York Academy of SCLence: 1997, pp 430–432.
Kessler R et al. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry 1995; 52: 1048–1060.
Solomon Z, Bleich A . Comorbidity of posttraumatic stress disorder and depression in Israeli veterans. Int J Neuro-psychiatr Med 1998; 3: 16–21.
Stein MB, Kennedy C . Major depressive and post-traumatic stress disorder comorbidity in female victims of intimate partner violence. J Affective Disorders 2001; 66: 133–138.
Maes M, Mylle J, Delmeire L, Altamura C . Psychiatric morbidity and comorbidity following accidental man-made traumatic events: incidence and risk factors. Eur Arch Psychiatry Clin Neurosci 2000; 250: 156–162.
Boekamp JR, Overholser JC, Schubert DSP . Depression following a spinal cord injury. Int J Psychiatry Med 1996; 26: 329–349.
Fuhrer MJ et al. Depressive symptomatology in persons with spinal cord injury who reside in the community. Arch Phys Med Rehabil 1993; 74: 255–260.
Kennedy P, Evans MJ . Evaluation of post-traumatic distress in the first 6 months following SCI. Spinal Cord 2001; 39: 381–386.
International standards for Neurological Classification of Spinal Cord injury. (Revised edn) American Spinal Injury Association (ASIA) and International Medical Society of Paraplegia (IMSOP): Chicago, IL 2000.
Mollica RF et al. The Harvard trauma questionnaire. Validating a cross-cultural instrument for measuring torture, trauma and posttraumatlc stress disorder in indochmese refugees. J Nerv Men Dis 1992; 180: 111–116.
Mollica RF et al. The dose–effect relationships between torture and psychiatric symptoms in Vietnamese ex-political detainees and a comparison group. J Nerv Ment Dis 1998; 186: 543–553.
Peltzer K . Ethno cultural constructions of posttraumatic stress symptoms in African contexts. J Psychol Afr 1998; 8: 17–30.
Mollica RF et al. Disability associated with psychiatric comorbidity and health status in Bosnian refugees living in Croatia. J Am Med Assoc 1999; 282: 433–439.
Overholser JC, Schubert DSP, Foliart R, Frost F . Assessment and emotional distress following a spinal cord injury. Rehabil Psychol 1993; 38: 187–198.
Tabachnick BG, Fidell LS . Using Multivanate Statistics. 4th edn. Allyn and Bacon: Needham Heights, MA 2000.
Radnitz CL et al. The prevalence of posttraumatic stress disorder in veterans with spinal cord injury. SCL Psychosoc Process 1995; 8: 145–149.
Richmond TS, Kauder D . Predictors of psychological distress following serious injury. J Traumatic Stress 2000; 13: 681–692.
Terr LC . Childhood traumas. An outline and overview. In: Horowitz MJ (ed). Essential Papers on Posttraumatic Stress Disorder. New York University Press: New York and London 1999, pp 61–81.
Emery VO et al. Predisposing variables in PTSD patients. J Traumatic Stress 1991; 4: 325–343.
Wilkeson A, Lambert MT, Frederick P . Posttraumatic stress disorder, dissociation, and trauma exposure in depressed and nondepressed veterans. J Nerv Ment Dis 2000; 188: 505–509.
Howell T, Fullerton DT, Harvey RF, Klein M . Depression in spinal cord injured patients. Paraplegia 1981; 19: 284–288.
Biering-Sørensen F, Pedersen W, Müller PG . Spinal cord injury due to suicide attempts. Paraplegia 1992; 30: 139–144.
Blanchard E, Buckley TC, Hickling EJ, Taylor AE . Posttraumatic stress disorder and comorbid major depression: is the correlation an illusion? J Anxiety Disorders 1998; 12: 21–37.
Franklin OL, Zimmerman M . Posttraumatic stress disorder and major depressive disorder: investigating the role of overlapping symptoms in diagnostic comorbidity. J Nerv Ment Dis 2001; 189: 548–551.
Lindemann E . Symptomatology and management of acute grief. Am J Psychiatry 1944; 101: 141–148.
Radnitz CL . Assessment of psychopathology and personality in people with physical disabilities. In: Frank RG, Elliott TR (eds). Handbook of Rehabilitation Psychology. American Psychological Association: Washington DC 2000.
Weisæth L . Importance of high response rates in traumatic stress research. Acta Psychiatr Scand Suppl 1989; 80: 131–137.
Acknowledgements
I am grateful to the patients at the Clinic for Paraplegia and Tetraplegia, Hornbæk, and Clinic for Paraplegia and Tetraplegia, Paraplegifunktionen, Viborg, for their participation, to the psychologists for their advice throughout the project, to Fin Biering-Sørensen for guidance concerning medical issues, to the secretaries for their practical help, and to the staffs in the rehabilitation centres for their assistance with this project.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Nielsen, M. Post-traumatic stress disorder and emotional distress in persons with spinal cord lesion. Spinal Cord 41, 296–302 (2003). https://doi.org/10.1038/sj.sc.3101427
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101427
This article is cited by
-
Post-traumatic stress disorder symptoms and pain intensity in persons with spinal cord injury
Spinal Cord (2021)
-
Increased psychological distress among individuals with spinal cord injury is associated with central neuropathic pain rather than the injury characteristics
Spinal Cord (2018)
-
Posttraumatic stress following spinal cord injury: a systematic review of risk and vulnerability factors
Spinal Cord (2017)
-
Event centrality as a unique predictor of posttraumatic stress symptoms and perceived disability following spinal cord injury
Spinal Cord (2017)
-
Depression, Posttraumatic Stress, and Risk Factors Following Spinal Cord Injury
International Journal of Behavioral Medicine (2014)